Abstract
Introduction: Secondary polycythemia (SP) is the increased number of red blood cells in the body that occurs due to elevated erythropoietin levels usually secondary to chronic hypoxia. Treating the underlying cause is the mainstay of treatment of SP. Phlebotomy is rarely used in patients with SP, especially those with symptoms related to hyperviscosity. We present a systematic review assessing the effectiveness of phlebotomy in SP.
Methods: Following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines, a comprehensive literature search was conducted on PubMed, Cochrane, and Clinical trials.gov using MeSH terms and keywords for "Polycythemia, Secondary " AND " Phlebotomy " in July 2022. We did not place any time constraints. Our search produced a total of 232 records, and duplicates were removed. After screening and removing irrelevant and review articles, we included a total of 17 original articles and case reports reporting phlebotomy as a treatment for SP in adult patients. The data were collected for baseline characteristics of the participants and efficacy and safety of the intervention.
Results:
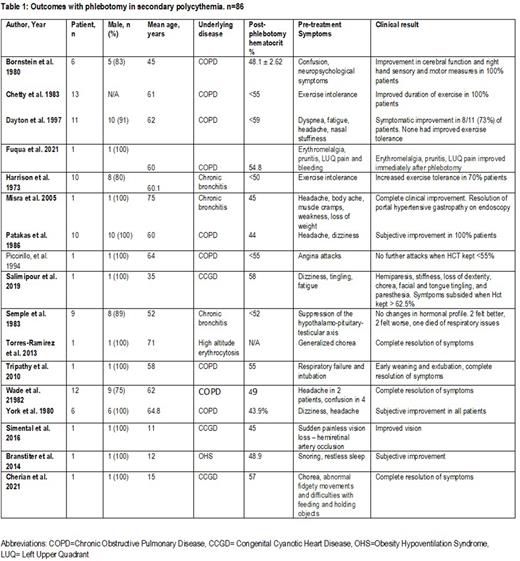
A total of 86 patients from 17 articles were evaluated. (Table 1) The mean age of participants was 51 years and 89% (n=65/73) were males. Most common cause of SP was chronic obstructive pulmonary disease (COPD) 94.4%, followed by congenital cyanotic heart disease (3.4%), high altitude erythrocytosis (1.1%), and obesity hypoventilation syndrome (1.1%). Most common reported symptoms were dyspnea, confusion, headaches, exercise intolerance, and suppression of hypothalamic-pituitary-testicular axis. Two case reports also reported chorea secondary to SP while there was one case report each for hemi-retinal artery occlusion, angina attacks and portal hypertensive gastropathy. Majority of the studies had a goal hematocrit of <55%. There was subjective improvement in clinical symptoms in 85% (n=73) of the patients while 2.3% (n=2) felt worse after phlebotomy. None of the patients (9/9) with suppression of hypothalamic-pituitary-testicular axis had improvement in hormonal profile after phlebotomy. One patient developed hemiparesis, stiffness, loss of dexterity, chorea after phlebotomy with the symptoms resolving when hematocrit went back to baseline >62.5%. One patient died a week after phlebotomy due to respiratory issues.
Conclusion: Phlebotomy results in clinical improvement in symptoms in patients with secondary polycythemia. Majority of the patients report either complete resolution of symptoms or at least subjective improvement. Goal hematocrit is usually <55%. Phlebotomy, although rarely used, may be considered a safe and effective treatment option for symptom management in SP, although its utility in objective improvement needs further prospective studies.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal